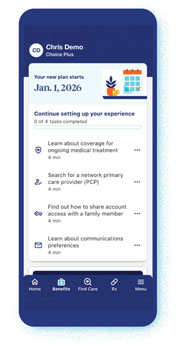
Take your next steps in the UnitedHealthcare app
With the UnitedHealthcare app, you'll see a variety of things you can do at your own pace which may help you get the most from your new plan the moment your coverage starts, which may include:
- Search for network providers
- Set up notifications and communication preferences
- Access on-demand, virtual assistance through the chat feature
- Start Transition of Care for ongoing treatment, if eligible
Keeping your care on track
When moving to a new plan, a little prep may help make the switch that much smoother. Let's walk through it together.
Deciding on your doctor
See the steps below if your provider is not in your new plan's network and you'd like to choose a new one — or if your plan requires you to have a PCP and you do not currently have one.
Choosing a new PCP
- Search your new plan’s provider network to find someone who feels like the right fit for you
- Once you’ve selected a PCP, make an appointment for after your new coverage begins — schedules can fill up so it’s usually good to do it early
- Request your medical records from your current provider — once you receive them, contact your new PCP to securely transfer
Even if your plan does not require you to have a PCP, it's a good idea to choose one — as your PCP is the doctor who understands your health needs and your health plan well.

Managing your meds
If your new plan involves drug coverage and if you're taking any medication, it's a good idea to complete these steps before your plan starts to avoid disruption.
- Fill any open prescriptions with your current pharmacy
- Search to see if your current pharmacy is included in your new plan’s network
- If they are, make sure they have your new plan information
- If they are not, search for a new network pharmacy and contact them to request a prescription transfer
- Search your new plan’s Prescription Drug List (PDL) to check if your meds are covered
- If they are covered, take note of your coverage levels to avoid surprises
- If they are not covered, talk with your provider right away about alternatives
Need more help or time to transfer medications?
Learn about Pharmacy Transition of Care (English) | (Spanish)

Continuing your care
If you’re actively receiving care for a qualifying condition from a provider who is not part of your new plan’s network, you may be able to keep seeing them for a limited time while you switch to a network provider. This is called Transition of Care.
Conditions that qualify may include, but are not limited to:
- Pregnancy and related care
- Ongoing cancer treatments
- Active care for a heart attack or stroke
- Certain surgeries or transplants
Conditions that do not qualify include, but are not limited to:
- Diabetes, arthritis, hypertension
- Routine exams and vaccinations
- Colds, sore throats, ear infections
- Certain elective surgeries
How to apply for Transition of Care
- Find and download the application form for your plan — this will include more details about eligibility specific to your plan
- If you’re unsure what type of plan you have, contact your employer or call the number on your health plan ID card, if you have it already
- Complete the form and get a signature from your current provider
- Submit the form within 30 days after your new plan’s start date to the address provided on the form

A new health care experience is waiting for you
Experience a health plan designed to be convenient and supportive, with opportunities to save.
Quality physicians and providers
Get recommendations for providers who may fit your needs and preferences
Benefits and rewards
Participate in programs and services designed to help you reach your health goals
Flexible access to care
Get access to care in a setting you prefer with digital, virtual and in-person options
Potential savings opportunities
Find cost-saving options, plus a cost estimator tool to help you plan and prepare
Dedicated member support
Connect to on-demand support that’s here to help along the way
Personalized digital tools
Tailor your digital experiences to match your preferences and help you make informed decisions
A closer look at transferring your care
Do you qualify for Transition of Care?
If you think you meet the requirements in the "Continuing your care" section above, call the number on your health plan ID card for assistance, if you have it already. Application forms may be specific to your plan, state, or employer.
Plan- and state-specific forms for Continuity of Care and Transition of Care
- FulIy Insured Transition of Care, Continuity of Care form (English)
- FulIy Insured Transition of Care, Continuity of Care form (Spanish)
- ASO Transition of Care, Continuity of Care form (English)
- ASO Transition of Care, Continuity of Care form (Spanish)
- Level Funded Transition of Care, Continuity of Care form (English)
- Level Funded Transition of Care, Continuity of Care form (Spanish)
For members who need help or more time to transfer medications, the Pharmacy Transition of Care flier (TOC) can help guide you.
Get answers to your questions
For open enrollment support, call 1-866-873-3903 or the number on your health plan ID card, if you already have it.
